Can excellent scientists be excellent physicians at the same
time?
“I would like to ask you about a trip to Thailand.”
This is not the kind of question I expected from a patient
in my cardiology clinic at the Veterans Administration hospital in
Indianapolis. Especially since this patient lived in rural Indiana and did not
strike me as the adventurous type.
“A trip to Thailand?”, I mumbled, “Well, ummm…I am
sure……ummm…I guess the trip will be ok. Just take your heart medications
regularly, avoid getting dehydrated and I hope you have a great vacation there.
I am just a cardiologist and if you want to know more about the country you
ought to talk to a travel agent.”
I realized that I didn’t even know whether travel agents
still existed in the interwebclickopedia world, so I hastily added “Or just use
a travel website. With photos. Lots of photos. And videos. Lots of videos.”
Now it was the patient’s turn to look confused.
“Doctor, I didn’t want to ask you about the country. I
wanted to know whether you thought it was a good idea for me to travel there to
receive stem cell injections for my heart.”
I was thrilled because for the first time in my work as a
cardiologist, a patient had asked me a question which directly pertained to my
research. My laboratory’s focus was studying the release of growth factors fromstem cells and whether they could help improve cardiovascular function. But my
excitement was short-lived and gradually gave way to horror when the patient
explained the details of the plan. A private clinic in Thailand was marketing
bone marrow cell injections to treat heart patients with advanced heart
disease. The patient would have to use nearly all his life savings to travel to
Thailand and stay at this clinic, have his bone marrow extracted and processed,
and then re-injected back into his heart in order to cure his heart disease.
Much to the chagrin of the other patients in the waiting
room, I spent the next half hour summarizing the current literature on
cardiovascular cell therapies for the patient. I explained that most bone marrow cells were not stem cells and that there was no solid evidence that he
would benefit from the injections. He was about to undergo a high-risk
procedure with questionable benefits and lose a substantial amount of money. I
pleaded with him to avoid such a procedure, and was finally able to convince
him.
I remember this anecdote so well because in my career as a
physician-scientist, the two worlds of science and clinical medicine rarely
overlap and this was one of the few exceptions. Most of my time is spent in my
stem cell biology laboratory, studying basic mechanisms of stem cell metabolism
and molecular signaling pathways. Roughly twenty percent of my time is devoted
to patient care, treating patients with known cardiovascular disease in
clinics, inpatient wards and coronary care units.
 |
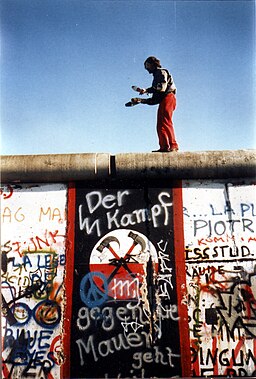
| “Portrait of Dr. Gachet” – Painting by Vincent van Gogh (Public Domain via Wikimedia) |
As scientists, we want to move beyond the current boundaries
of knowledge, explore creative ideas and test hypotheses. As physicians, we
rely on empathy to communicate with the patient and his or her family, we apply
established guidelines of what treatments to use and our patient’s comfort
takes precedence over satisfying our intellectual curiosity. The mystique of
the physician-scientist suggests that those of us who actively work in both
worlds are able to synergize our experiences from scientific work and clinical
practice. Being a scientist indeed has some impact on my clinical work, because
it makes me evaluate clinical data on a patient and published papers more
critically. My clinical work helps me identify areas of research which in the
long-run may be most relevant to patient care. But these rather broad forms of
crosstalk have little bearing on my day-to-day work, which characterized by
mode-switching, vacillating back and forth between my two roles.
Dr. J. Michael Bishop, who received the Nobel Prize in 1989
with Dr. Harold Varmus for their work on retroviral cancer genes (oncogenes),
spoke at panel discussion at the 64th Lindau Nobel Laureate Meeting (2014) about
the career paths of physician-scientists in the United States. Narrating his
own background, he said that after he completed medical school, he began his
clinical postgraduate training but then exclusively focused on his research.
Dr. Bishop elaborated how physician-scientists in the United States are often
given ample opportunities and support to train in both medicine and science,
but many eventually drop out from the dual career path and decide to actively
pursue only one or the other. The demands of both professions and the financial
pressures of having to bring in clinical revenue as well as research grants are
among the major reasons for why it is so difficult to remain active as a
scientist and a clinician.
To learn more about physician-scientist careers in Germany,
I also spoke to Dr. Christiane Opitz who heads a cancer metabolism group at the
German Cancer Research Center, DKFZ, in Heidelberg and is an active clinician.
She was a Lindau attendee as a young scientist in 2011 and this year has
returned as a discussant.
JR: You embody the physician-scientist role, by actively
managing neuro-oncology patients at the university hospital in Heidelberg as
well as heading your own tumor metabolism research group at the German Cancer
Research Center (Deutsches Krebsforschungszentrum or DKFZ in Heidelberg). Is
there a lot of crosstalk between these two roles? Does treating patients have a
significant influence on your work as a scientist? Does your work as cancer
cell biologist affect how you evaluate and treat patients?
CO: In my experience, my being a physician influences me on
a personal level and my character but not so much my work as a scientist. Of
course I am more aware of patients’ needs when I design scientific experiments
but there is not a lot of crosstalk between me as a physician and me as a
scientist. I treat patients with malignant brain tumors which is a fatal
disease, despite chemotherapy and radiation therapy. We unfortunately have very
little to offer these patients. So as a physician, I see my role as being there
for the patients, taking time to talk to them, provide comfort, counseling
their families because we do not have any definitive therapies. This is very
different from my research where my aim is to study basic mechanisms of tumor
metabolism.
There are many days when I am forced to tell a patient that
his or her tumor has relapsed and that we have no more treatments to offer. Of
course these experiences do motivate me to study brain tumor metabolism with
the hope that one day my work might help develop a new treatment. But I also
know that even if we were lucky enough to uncover a new mechanism, it is very
difficult to predict if and when it would contribute to a new treatment. This
is why my scientific work is primarily driven by scientific curiosity and
guided by the experimental results, whereas the long-term hope for new
therapies is part of the bigger picture.
JR: Is it possible that medical thinking doesn’t only help
science but can also be problematic for science?
CO: I think in general there is increasing focus on
translational science from bench-to-bedside, the aim to develop new treatments.
This application-oriented approach may bear the risk of not adequately valuing
basic science. We definitely need translational science, because we want patients
to benefit from our work in the basic sciences. On the other hand, it is very
important to engage in basic science research because that is where – often by
serendipity – the real breakthroughs occur. When we conduct basic science
experiments, we do not think about applications. Instead, we primarily explore
biological mechanisms.
Physicians and scientists have always conducted
“translational research”, but it has now become a very popular buzzword. For
that reason, I am a bit concerned when too much focus and funding is shifted
towards application-oriented science at the expense of basic science, because
then we might lose the basis for future scientific breakthroughs. We need a
healthy balance of both.
JR: Does the medical training of a physician draw them
towards application-oriented translational science and perhaps limit their
ability to address the more fundamental mechanistic questions?
CO: In general, I would say it is true that people who were
trained purely as scientists are more interested in addressing basic mechanisms
and people who were trained as physicians are more interested in understanding
applications such as therapies, therapeutic targets and resistance to
therapies.
They are exceptions, of course, and it is ultimately
dependent on the individual. I have met physicians who are very interested in
basic sciences. I also know researchers who were trained in the basic sciences
but have now become interested in therapeutic applications.
JR: When physicians decide to engage in basic science, do
you think they have to perhaps partially “unlearn” their natural tendency of
framing their scientific experiments in terms of therapeutic applications
because of their exposure to clinical problems?
CO: We obviously need application-oriented science, too. It
is important to encourage physicians who want to pursue translational research
in the quest of new therapies, but we should not regard that as superior to
basic science. As a physician who is primarily working in the basic sciences, I
make a conscious effort to focus on mechanisms instead of pre-defined
therapeutic goals.
Looking to the future
Dr. Opitz’s description of how challenging it is to navigate
between her clinical work in neuro-oncology and her research mirrors my own
experience. I have often heard that the physician-scientist is becoming an
“endangered species”, implying that perhaps we used to roam the earth in large
numbers and have now become rather rare. I am not sure this is an accurate
portrayal. It is true that current financial pressures at research funding
agencies and academic institutions are placing increased demands on
physician-scientists and make it harder to actively pursue both lines of work.
However, independent of these more recent financial pressures, it has always
been extremely challenging to concomitantly work in two professions and be good
at what you do. Dr. Bishop decided to forsake a clinical career and only focus
on his molecular research because he was passionate about the research. His
tremendous success as a scientist shows that this was probably a good decision.
As physician-scientists, we are plagued by gnawing
self-doubts about the quality of our work. Can we be excellent scientists and
excellent physicians at the same time? Even if, for example, the number of days
we see patients are reduced to a minimum, can we stay up-to-date in two
professions in which a huge amount of new knowledge is produced and published
on a daily basis? And even though the reduction in clinical time allows us to
develop great research programs, does it compromise our clinical skills to a
point where we may not make the best decisions for our patients?
We are often forced to sacrifice our week-ends, the hours we
sleep and the time we spend with our families or loved ones so that we can cope
with the demands of the two professions. This is probably also valid for other
dual professions. Physician-scientists are a rare breed, but so are
physician-novelists, banker-poets or philosopher-scientists who try to remain
actively engaged in both of their professions.
There will always be a rare population of
physician-scientists who are willing to take on the challenge. They need all
the available help from academic institutions and research organizations to
ensure that they have the research funds, infrastructure and optimized work
schedules which allow them to pursue this extremely demanding dual career path.
It should not come as a surprise that, despite the best support structure, a
substantial proportion of physician-scientists will at some point feel
overwhelmed by the demands and personal sacrifices and opt for one or the other
career. Even though they may choose drop out, the small pool of
physician-scientists will likely be replenished by a fresh batch of younger
colleagues, attracted by the prospect of concomitantly working in and bridging
these two worlds.
Instead of lamenting the purported demise of
physician-scientists, we should also think about alternate ways to improve the
dialogue and synergy between cutting-edge science and clinical medicine. A
physician can practice science-based medicine without having to actively work
as a scientist in a science laboratory. A scientist can be inspired or informed
by clinical needs of patients without having to become a practicing physician.
Creating routine formalized exchange opportunities such fellowships or
sabbaticals which allow scientists and clinicians to spend defined periods of
time in each other’s work environments may be much more feasible approach to
help bridge the gap and engender mutual understanding or respect.
Originally published as “Physician Scientists: An Endangered Species?“ in the Lindau Nobel Laureates Meeting blog.